The Center for Brain/Mind Medicine > Support & Education
End of Life With Dementia
There will come a time on the dementia journey when the end is near. Thinking about this milestone and the subject of death itself can bring up many emotions, including fear, discomfort, avoidance, sadness, overwhelm, and even relief. This is all normal. As a caregiver, you’ve experienced changes in care that evolved as the disease progressed. The end of life is a challenging time for the person and those around them. It can also be a time for connection, healing, and support for your person, yourself, and others. Planning for the end of life and communicating to key family members and friends is important for anyone who has a life-limiting condition. For a person with dementia, it’s important to have these conversations early, while it is still possible to make shared decisions. Below you will find information about this stage of the dementia journey that we hope you will find helpful as you prepare for the future.
Review of Late-Stage Dementia
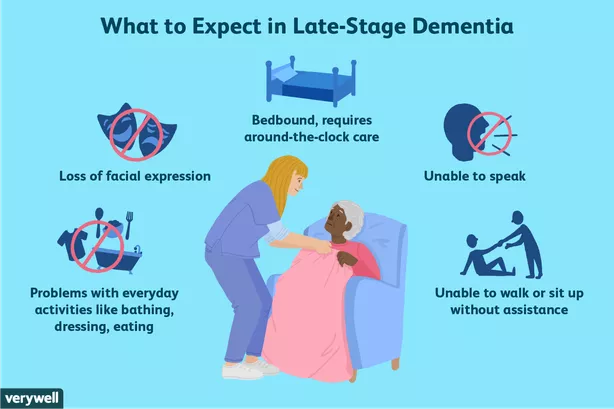
In the late stage of the disease, we continue to see declines in the person’s memory and overall functioning, including:
- Verbal communication—more reliant on non-verbal language, grunts and groans, and behaviors.
- Physical abilities—decreased participation in daily care (including bathing and toileting/incontinence), inability to walk on their own (or becoming bed-bound), and/or difficulty eating (using fingers instead of utensils, having trouble with swallowing), sleeping more.
- Memory—does not recognize us or other immediate family members or close friends.
- Increased risk for other medical complications—infections such as Urinary Tract Infections (UTIs) and pneumonia, skin breakdown, blood clots, falls, dehydration, and malnutrition.
You can expect that during this stage, your person will need more oversight and hands-on care—most likely around-the-clock care.
What to Expect at the End of Life
Given the variability within dementia’s progression for each person, it can be difficult to know when someone with dementia is nearing the end of life. Additionally, people may have other chronic health conditions that are being monitored and managed and that may cause death before dementia does. The end of life is a time when decision-making related to care can be at the forefront as you work toward keeping your person as comfortable as possible. As caregivers, becoming informed about what to expect nearing or at the end of life and what care options are available is important to ensure that the person with dementia receives needed care.
The timeline of what you might see in the last six months of life, and even in the days and weeks before death, varies. Some of the key signs that the end of life is near include the body’s organs and systems shutting down, reduction in consciousness, and periods of restlessness and agitation. In the end, many people with late-stage dementia die of medical complications related to the underlying dementia. For instance, a person may pass from an infection like aspiration pneumonia (which can be a result of swallowing difficulties), sepsis (which can occur due to a UTI), or a blood clot in the lung (as a result of being immobile and bed-bound). It’s important to note that many persons with dementia die of other causes before death from dementia occurs.
Care Considerations for Late-Stage Dementia & the End of Life
As a result of the decline in late-stage dementia and co-occurring medical conditions common in later life, there are often increased urgent-care or emergency-room visits, along with increased risk of caregiver burden and fatigue. During these acute periods of illness, caregivers may be faced with decision-making around care interventions. Aggressive medical approaches at this stage may not only be of limited value, but may be detrimental to the quality of life and comfort of the person with dementia. Caring for persons with dementia in the late stage and at the end of life usually involves difficult decisions about treatment goals. It’s not uncommon for some primary caregivers and family members to feel a great deal of guilt and/or ambivalence about these decisions.
A good first step when we consider the end of life and late-stage dementia is becoming familiar with important documents and care options that might be helpful in advance of need. This way you will have a greater understanding of when to incorporate these options and tools into your person’s care. Important documents include MOLST (Medical Order for Life-Sustaining Treatment), Health Care Proxy (HCP), Living Will, and Durable Power of Attorney. Care options may include Palliative Care and Hospice.
Important Documents
MOLST | Health Care Proxy | Living Will | Durable Power of Attorney | Last Will & Testament | |
| Type | Medical order | Legal document | Legal document | Legal document | Legal document |
| Form Users | Patients of any age with advanced illness | All adults, healthy or ill | All adults, healthy or ill | All adults, healthy or ill | All adults, healthy or ill |
| Purpose | A medical order communicating decisions regarding life-sustaining treatment (resuscitation, ventilation, transport to hospital, dialysis, and artificial nutrition and hydration); most often used in emergency situations | Appoints a trusted person to be health care agent, to make medical and mental health decisions on person’s behalf should they be unable to do so | Instructs HCP and medical providers of wishes related to medical treatments and directions about what the person does and does not want; organ and tissue donor wishes, and spiritual and religious considerations | Appoints a trusted person to manage money, property, and financial matters; can specify limited or general powers | Informs of asset distribution, names an executor, nominates guardian for any dependents |
| Form signer(s) | Patient or representative and medical provider | Person and two witnesses of the person’s choice | Patient/person | Patient/person, advisable to complete with attorney | Person, testator, and two witnesses |
| In Effect? | Immediately upon signing | After a patient is declared incapable of making medical decisions by a doctor | When a patient is unable to speak for themselves | Immediately upon signing | Immediately upon signing |
NOTE: Different states have different rules around advance directives and legal documents. Seek legal counsel to learn more.
Differences Between Palliative Care & Hospice
Palliative Care | Hospice | |
| What is the focus of care? | Focuses on quality of life and advance-care planning at any stage of a serious illness | Focuses on managing pain, symptoms, and stress of serious illness during the terminal phase; additionally, provides emotional and spiritual support to patients and families |
| Who can receive services? | Anyone with a serious or chronic illness at any stage; eligibility not based on life expectancy | Anyone who has a life-limiting condition and a life expectancy of six months or less |
| Can curative treatments be continued? (chemotherapy, radiation, dialysis, surgery, rehab therapies) | Yes—curative treatments and those intended to prolong life can be continued | No—hospice is available to people who are no longer seeking curative treatment and whose focus is comfort |
| What services are provided? | Pain and symptom management, in-person and telephone visits, help navigating treatment options, advance-care planning, and referrals to community resources | Pain and symptom management, 24-hour on-call service, in-person visits, medical equipment, medications, respite care, volunteer services, spiritual care, and bereavement counseling |
| Who provides these services? | The palliative care team may include a physician and/or nurse practitioner, social worker, and/or chaplaincy services. This team works in collaboration with the existing medical team. | The hospice team is interdisciplinary, including a hospice physician, nurse case manager, hospice aide, social workers, chaplain, bereavement counselor, and trained volunteers. The hospice team will take the lead with medical interventions from the time of enrollment. |
| Where can I receive these services? | Visits are provided at home, assisted living community, hospital (consult service), or skilled nursing facility | Care is provided where the patient is located—in their own home, assisted living community, skilled nursing facility, hospital, or hospice home (facilities need to be licensed for hospice care) |
| What are the payment sources for these services? | Medicare Part B, MassHealth, and some private insurance plans; all may be subject to co-pay according to plan | Covered for most patients by Medicare Part A, Medicaid, and most private insurance |
| When should I consider signing up for this service? | At any stage of a serious illness, including dementia | When there is a prognosis of 6 months or less and no more engagement in curative treatment; a physician must certify prognosis |
Speak with your person’s primary care physician and/or neurologist if you are interested in learning more about palliative care and/or hospice services and when these might be a good fit.
How You Can Help at the End of Life
- Continue to provide your person with love and support. Click here for suggestions on ways to comfort your person at the end of life.
- Because your person may be unable to communicate with words, monitor them for any signs of pain or discomfort, such as moaning, restlessness, inability to sleep, pained facial expression, or sweating.
- Ongoing collaboration with your person’s medical team around goals of care and medical interventions is of utmost importance.
- Review the Health Care Proxy and the person with dementia’s Living Will (if completed in advance). Late-stage dementia and the end of life may require medical decision-making on behalf of your person. It will be helpful for the Health Care Proxy and those involved with care to review the person’s wishes relating to care decisions and comfort measures.
- If not already in place, and as you are able, consider funeral planning in advance of your person’s passing. This can be an act of compassion for yourself so you do not have to make these decisions in a time of crisis.
Learn More
BWH Health Care Proxy and Living Will (Printable Forms)
Caring for Someone at the End of Life – National Institute of Nursing Research
The Conversation Project
End of Life Decisions pamphlet – Alzheimer’s Association
End of Life Guideline Series: A Compilation of Barbara Karnes Booklets
Honoring Choices Massachusetts
Locate a Palliative Care or Hospice agency servicing your town here.
Reference BWH handout, “Ways to Provide Comfort at End of Life”
Consider linking with a bereavement support group—often offered through the hospice care agency.